Thoracolumbar Spine
Special Questions
- Bowel / Bladder dysfunction
- Loss of weight / appetite
- Weakness / clumsiness / gait disturbance
- Pins and Needles or numbness
- Recent spinal surgery
- History of malignancy
-
Red Flags
- Infection
- Fever / other signs of infection
- Underlying disease process, immunosuppression, penetrating wound
- History of IV drug use
- Fracture
- History of Trauma (or minor trauma if >50 and with history of OP +/- prolonged steroid use)
- Tumour
- Past History of malignancy
- Age >50
- Failure to improve with Rx
- Unexplained LOW
- Pain at multiple sites +/- resting pain
- AAA
- Absence of aggravating factors
- Infection
- Presence of leg pain
Goals in ED
Neuromeningeal Testing





 A strong stretch is normal – reproduction of the patient’s pain is abnormal
A strong stretch is normal – reproduction of the patient’s pain is abnormal
Neurological Examination
Palpation
Other Tests
Imaging
Yellow Flags
- Normal distal neurovascular function
- Not a non-musculoskeletal cause
- No fractures / dislocations
- No gross neurological dysfunction or other signs / symptoms suggestive of cauda equina or other sinister pathology
Standing Assessment
- Observation
- Rash / Swelling
- Posture
- Presence of a list (note which direction pelvis is shunted)
- Active Range of Motion (if possible)
- Standing
- Flexion
- Extension
- Lateral Flexion
- Seated
- Rotation
- Standing
- Gait
Bed Assessment
Neuromeningeal Testing
- This involves stretching the tissues that protect the central and peripheral nervous system
- If there is tethering of neural structures (eg from a nerve root compression, scar tissue from an injured muscle or laceration sticking to peripheral nerves), stretching of these structures usually reproduces pain
- A positive test does not necessarily mean that the pain is coming from compression of nerve roots – it merely indicates that SOME component of the pain is relating to the neuromeningeal structures
- Prone knee bend stresses the anterior travelling nerve fibres
- Begin by flexing the patient’s knee to 90 degrees

- Extend the patient’s hip from the bed until they tell you to stop, significant pain is elicited or there is no further range possible

- A strong stretch is normal – reproduction of the patient’s pain is abnormal
- Measure the angle at which symptoms are first produced
- The straight leg raise test for LBP is PASSIVE (active straight leg raising pulls anteriorly on the lumbar spine via Psoas and will reproduce lower back pain in most patients).

- Straight leg raise stresses the posteriorly travelling nerves (which terminate in the sole of the foot)

- Begin by dorsiflexing the patient’s foot

- Keeping the knee straight, lift the patient’s leg from the bed until they tell you to stop, significant pain is elicited or there is no further range
 A strong stretch is normal – reproduction of the patient’s pain is abnormal
A strong stretch is normal – reproduction of the patient’s pain is abnormal
- Measure the angle at which symptoms are first produced
- Move the ankle into plantarflexion and note any changes in pain
- SLR is highly sensitive for herniated discs (0.92), but of variable specificity (0.1 to 1)
- Crossed SLR (eg SLR on L causes pain on R) shows high specificity (0.9) but low sensitivity (0.28) * Surgical population
- Prone Knee Bend
- * Slump (generally not needed unless trying to clear lumbar spine)
Neurological Examination
- Power
- Explain to the patient that you understand that it may be uncomfortable to push, however this is an important part of the assessment. Advise the patient to put the pain aside and push against you as hard as they possibly can.
- Measure using the Oxford grading system:
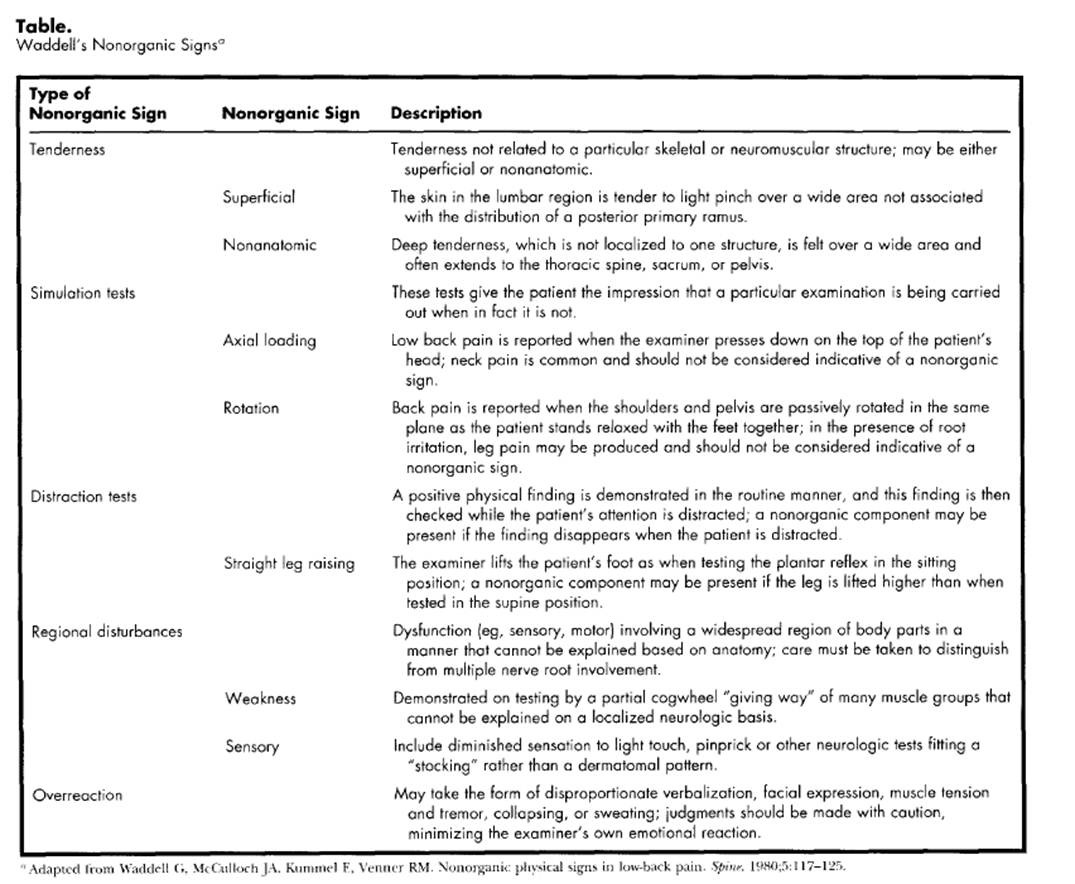
| Oxford Grade | Descriptor |
|---|---|
| 0 | No signs of activity |
| 1 | Flicker of activity, no movement |
| 2 | Full active range of motion, across gravity |
| 3 | Full active range of motion, against gravity |
| 4 | Moderate resistance |
| 5 | Maximal resistance |
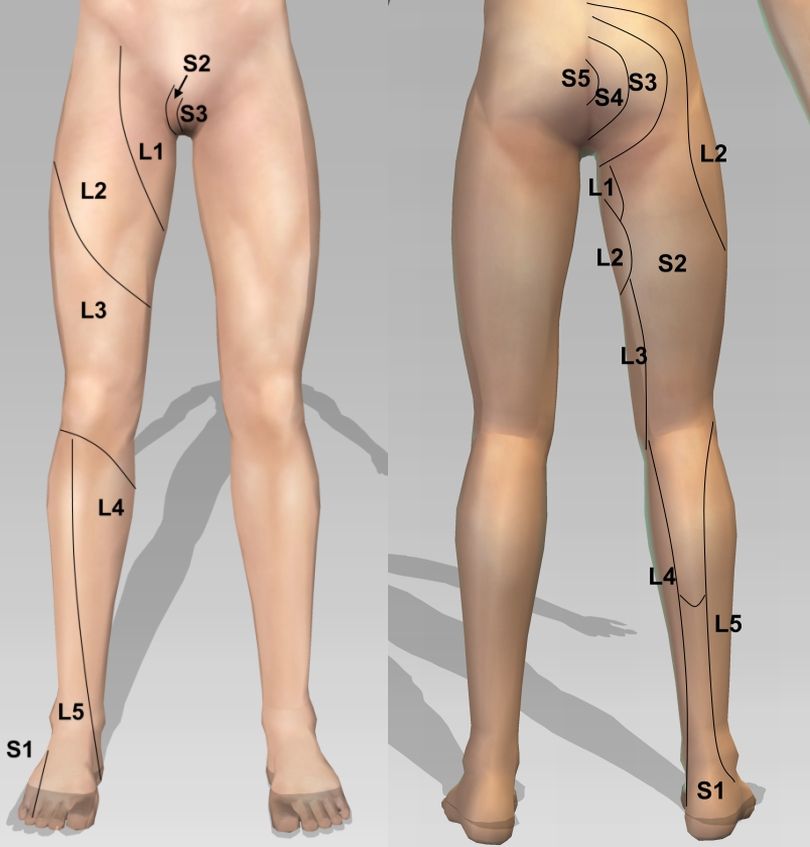
- Myotomes
- Hip flexion (L2/3)
- Knee extension (L3/4)
- Ankle DF (L4/5)
- Great toe ext (L5)
- Ankle PF (S1/S2)
- Reflexes
- Technique
- Patient must be relaxed
- Grip on hammer should be loose (hammer should bounce when striking tendon)
- Compare to normal side (or knowledge of “normal”)
- Abnormalities
- Hypoactive (nerve root)
- Hyperactive (cord / CNS)
- Grading
- No response
- + = lower than normal
- ++ = normal
- +++ = brisk
- ++++ = very brisk
- Clonus
- Specific Reflexes
- Knee Jerk (L3/4)
- Ankle Jerk (S1/S2)
- Plantars (UMN vs LMN)
- Technique
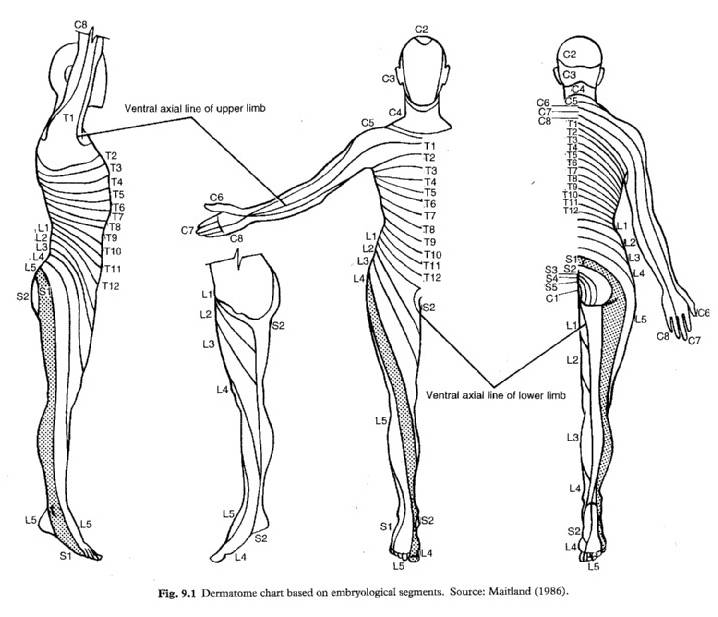
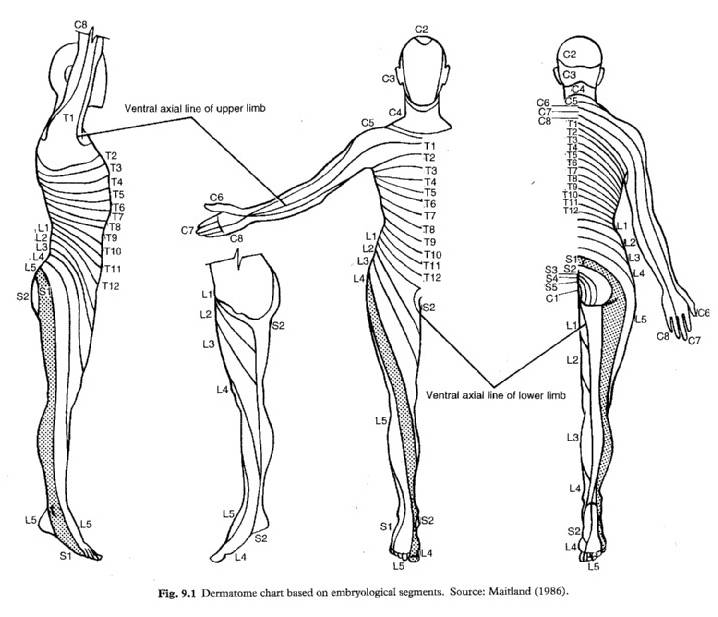
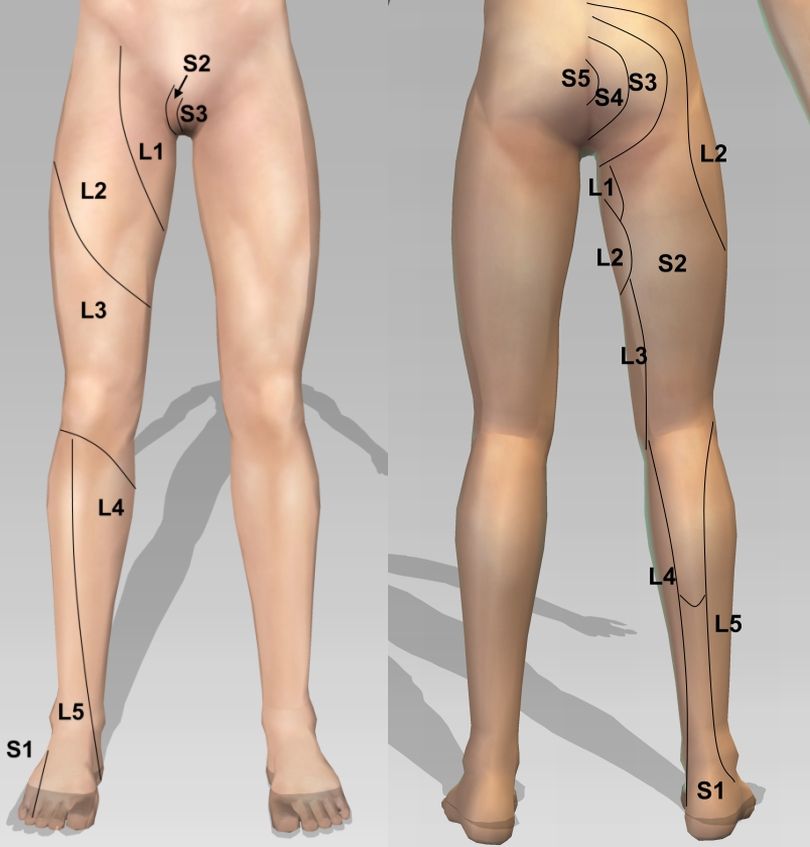
- Sensation
- Dermatomal (including perianal)
- *Coordination (if seems more like a SYSTEMIC neurological problem rather then a SPINAL neurological problem)
- Heel shin
- Gait
Palpation
- Thoaco-Lumbar spine
- Flank
Other Tests
- Obs – HR, BP, Temp, O2 sat
- Full Ward Test (urine) if potential for UTI / renal colic / other cause for pain
- Post Void Residual Volume (bladder scan in ED to check if is in urinary retention) if incontinence / retention
- Considered abnormal if PVRV > 100mls
Imaging
- X-ray
- Trauma in younger patients
- Minimal trauma in frail older patients
- Hx of malignancy
- Other red flags (LOA / LOW / Bowel / Bladder)
- CT / MRI (need to discuss with specialty registrar)
- Significant neurological dysfunction
- Gross motor changes
- Urinary retention / incontinence
- Gait disturbance
- Significant neurological dysfunction
Yellow Flags