Deciding to Image (Knee)
The Ottawa Knee Rule states that for patients with an acute knee injury, a knee x-ray is ONLY indicated if ANY of the following criteria are met:
 There are also the Pittsburgh Knee Rules, which state that radiographs of the knee should performed if the mechanism of injury is a fall or blunt trauma and at least one of the following:
There are also the Pittsburgh Knee Rules, which state that radiographs of the knee should performed if the mechanism of injury is a fall or blunt trauma and at least one of the following:
- Aged > 55 years
- Inability to flex the knee to 90 degrees
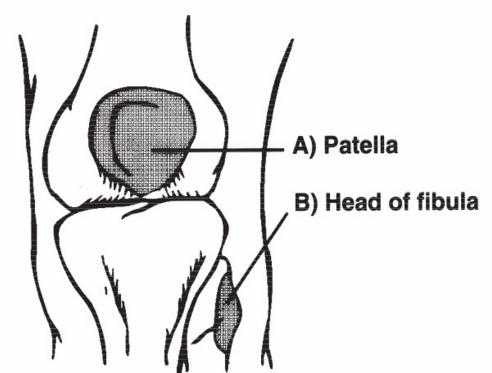
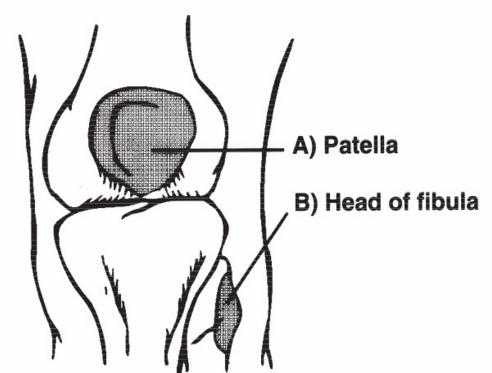
- Isolated tenderness to the patella
- Tenderness to the fibular head
- Inability to weightbear for 4 steps (regardless of limp) both immediately and on assessment
 There are also the Pittsburgh Knee Rules, which state that radiographs of the knee should performed if the mechanism of injury is a fall or blunt trauma and at least one of the following:
There are also the Pittsburgh Knee Rules, which state that radiographs of the knee should performed if the mechanism of injury is a fall or blunt trauma and at least one of the following:
- Patient is younger than 12 or older than 50
- Inability to walk four weight-bearing steps
- More than 6 days after injury
- Those with only superficial lacerations and abrasions
- Previous history of knee injury or surgery on the affected knee
- Being reassessed for the same injury
- MSK Ultrasound is generally not of great use in the Emergency Department UNLESS you are suspicious of a quadriceps / patellar tendon injury with ambiguous other objective findings.
- MSK Ultrasound cannot adequately image the menisci or cruciate ligaments, and while they can visualise the collateral ligaments, clinical assessment can give this information (and more) and even substantial damage to the collateral ligaments would not necessitate urgent surgery.
- Doppler Ultrasound can be of use if there is suspicion of Deep Vein Thrombosis
- The Well's criteria is a tool which can be used to predict DVT and determine further investigation.
- Wells score or criteria: (possible score −2 to 9)
- Active cancer (treatment within last 6 months or palliative): +1 point
- Calf swelling ≥ 3 cm compared to asymptomatic calf (measured 10 cm below tibial tuberosity): +1 point
- Swollen unilateral superficial veins (non-varicose, in symptomatic leg): +1 point
- Unilateral pitting edema (in symptomatic leg): +1 point
- Previous documented DVT: +1 point
- Swelling of entire leg: +1 point
- Localized tenderness along the deep venous system: +1 point
- Paralysis, paresis, or recent cast immobilization of lower extremities: +1 point
- Recently bedridden ≥ 3 days, or major surgery requiring regional or general anesthetic in the past 12 weeks: +1 point
- Alternative diagnosis at least as likely: −2 points
- Those with Wells scores of two or more have a 28% chance of having DVT, those with a lower score have 6% odds. Alternatively, Wells scores can be categorized as high if greater than two, moderate if one or two, and low if less than one, with likelihoods of 53%, 17%, and 5%, respectively.
- If there is a low probability of DVT, but suspicion has been raised, then d-dimer testing is recommended to exclude a DVT
- If d-dimer is elevated or is there is a moderate or high probability of DVT using the Well's criteria, then doppler ultrasound is required
- CT scanning is useful in the ED setting for musculoskeletal injuries to:
- Identify fractures where there is strong suspicion, but no definite fracture on plain imaging
- To quantify fractures to provide assistance for further management (eg for orthopaedic surgery)
- MRI is useful for imaging significant soft tissue injuries which may require prompt attention as well, such as a grossly unstable knee.
Knee Injuries
Patella Fracture

- Stable, undisplaced and minimally displaced fractures of the patella are managed in a Zimmer Splint for approximately 6 weeks, keeping the knee completely straight.
- Straight leg raising can assist in indicating the stability of patellar fractures (although if both the retinaculi are intact, it is possible to be able to straight leg raise with a displaced patellar fracture as witnessed by the author). Pain may also prevent straight leg raising in the presence of a stable patella fracture (quadriceps function might need to be assessed in a different position)
- Displaced patella fractures require operative management.

- A Segond fracture is a small avulsion type fracture of the lateral aspect of the tibial plateau where the lateral capsular ligament avulses a fragment of bone. It is NOT from the Lateral Collateral Ligament, which attaches to the fibular head.
- While the significance of the actual fracture is not great (conservative management), the presence of a Segond fracture is almost always (95%) accompanied by an ACL rupture and often by a medial meniscal tear as well (up to 60%)

- In the skeletally immature patient, the tibial tubercle may be avulsed by the pull of the patella tendon.
- This is usually the culmination of repeated trauma and the patient will often have a history of Osgood Schlatter’s “disease”.
- Treatment depends on level of displacement, ranging from immobilisation in an extension splint for stable, minimally displaced injuries to ORIF for significantly displaced fractures

- The Anterior Cruciate Ligament attaches to the anterior tibial spine (which is the most lateral on an AP x-ray) and the Posterior Cruciate Ligament to the posterior tibial spine (which is the most medial on an AP x-ray)
- In this film, the ACL has avulsed the anterior tibial spine.
- Note the presence of a lipohaemarthrosis on the Horizontal Beam view. Fat visible on x-ray usually indicates fracture. The five causes of a haemarthrosis are intra-articular fracture, ACL rupture, PCL rupture, meniscal tear and PFJ dislocation.
- On CT scan, these injuries often look significantly worse than they do on plain film and are usual practice to further evaluate
- Management usually entails surgery unless undisplaced.

- Tibial plateau fractures vary significantly in their appearance.
- This film shows an obviously displaced tibial plateau fracture which requires ORIF, however these are often subtle, with varying amounts of depression seen on AP films.

- Depressed fracture of the medial tibial plateau, also requiring ORIF.
- If the fracture is only minor, with minimal depression, management may not require surgery and just NWB for a length period with some sort of immobilisation (HKB or ZKS)
- The Maisonneuve fracture is a spiral fracture of the upper third of the fibula associated with a tear of the distal tibiofibular syndesmosis and the interosseous membrane.
- There is an associated fracture of the medial malleolus or rupture of the deep deltoid ligament.
- These injuries need orthopaedic attention as they are inherently unstable
- In contrast, an isolated fibular neck fracture associated with a direct blow is often managed symptomatically.